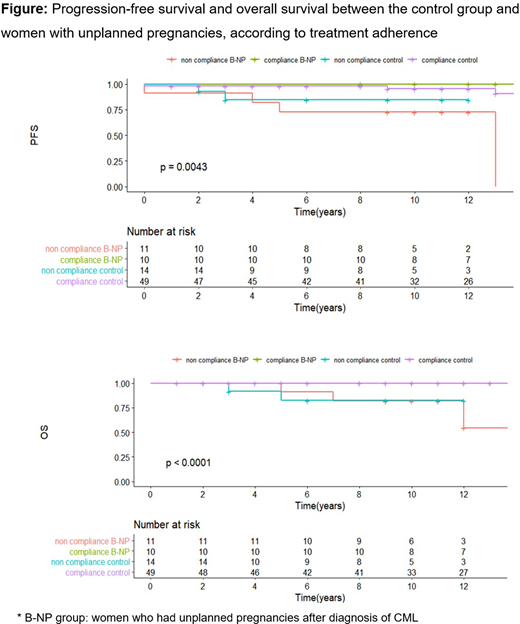
The management of chronic myeloid leukemia (CML) during pregnancy is a subject of continuous debate and there are few reports on CML outcomes in these women. The aim of the study is to compare progression-free survival (PFS) and overall survival (OS) between women who became pregnant after the diagnosis of CML and those who did not, as well as describing the treatments performed during pregnancy and maternal-fetal outcomes.Methods:Retrospective study, including women under 45 years of age and diagnosis of CML between 1991 and 2018, from the database of the Clinical's Hospital of the University of Medical School of São Paulo and the Cancer Institute of the State of São Paulo-Brazil.Results:100 cases were reviewed and 98 were included for analysis. The PFS and OS of groups A (63 non-pregnant women) and B (35 pregnant women, totaling 46 pregnancies) did not show statistical difference in a median of 11 years of follow-up (p=0.15). In the multivariate analysis, only poor adherence to treatment was identified as an independent risk factor for PFS and OS (HR: 9.7, 95% CI: 1.9-47.7). Comparing women with unplanned pregnancies (group B-UP, n= 21) with group A and considering adherence, PFS was worse in group B-UP without adherence (p<0.0001). The non-adherence rate in groups A, B and B-UP was 22%, 40% and 52%, respectively. Of the women who received treatment during pregnancy (60%), 2 underwent leukapheresis, 18 received alpha interferon (IFN) and 1 hydroxyurea. Among those who had a major molecular response/ deep molecular response at the beginning of pregnancy and discontinued the Tyrosine Kinase Inhibitor (ITK), 63% lost response and of these, 90% recovered after reintroduction. None evolved with progression or death. Complications occurred in 37% of all pregnancies: 9 abortions, 3 premature, 3 hypertensive disordes of pregnancy, 1 placental abruption and 1 fetal distress. The conception occurred in the presence of ITK in 60% of pregnancies and 52% of them evolved with complications, including 2 fetal malformations (encephalocefele with absence of cerebellar vermis and hydrocele).Discussion:Literature is scarce regarding the outcome of CML in women who become pregnant. This is the first study that evaluates pregnancy as a risk factor for progression/death, comparing pregnant women and non-pregnant women in the same cohort. Although pregnancy does not have an impact on outcomes, women who have unplanned pregnancies have a greater chance of non-adherence and, consequently, worse PFS. Several studies have already observed that non-adherence to treatment increases the chance of treatment failure, as well as the risk of progression. However, there are no reports that unplanned pregnancies are alert for non-adherence. The rate of loss of response and its recovery after reintroducing the ITK was similar to that found in the literature. With the current possibility of maintaining remission after treatment interruption, it opens up possibilities for planning pregnancy since the beginning of the diagnosis of CML. There is no consensus on the best treatment of CML during pregnancy, but leukapheresis and IFN are known to be safe; while hydroxyurea and ITK should be avoided due to the risk of teratogenicity and pregnancy complications.Conclusion:Pregnancy itself does not interfere with long-term outcomes of CML, however, women who have an unplanned pregnancy are at increased risk of non-adherence, as well as progression and death due to CML and deserve a special approach.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal